What is vaginismus/ GPPD?
Vaginismus is vaginal tightness resulting from the involuntary tightening of the pelvic floor muscles, causing discomfort, burning, pain, penetration problems, or even the complete inability to have intercourse. Vaginismus is also known as genito-pelvic pain disorder or genito-pelvic penetration disorder (GPPD), pelvic floor over-activity/hypertonicity, pelvic floor myalgia, and is sometimes confused with vulvodynia.
Having primary vaginismus means you experienced vaginismus from your very first attempt of intercourse, and perhaps you have never been able to use tampons or complete a vaginal examination or Pap smear at the doctor’s. Having secondary vaginismus means that you have previously been able to enjoy pain-free intercourse but then experienced vaginismus at a later stage, for example after an infection, childbirth or surgery.
The exact number of women with vaginismus is difficult to know, but in clinical settings, the rates are reported to be between 5-17% (Lahaie et al, 2010; Melnik et al, 2012). If you have experienced vaginismus, you are certainly not alone.
What causes vaginismus/ GPPD?
Vaginismus is a unique condition in that it may result from a combination of either physical or non-physical causes or it may seem to have no cause at all.
Titration is best done with short-acting heroin. Its action begins in an hour and lasts for 4 hours. If the effect does not occur within an hour, the dose should be repeated. In the case of titration of extended-release morphine, it takes 4 hours to see the full effect of this drug.Extended-release drugs are recommended when the amount of morphine has been titrated. If only extended-release morphine is available for titration, then dose selection will take longer.
Examples of Physical Causes:
Poor muscle recruitment The pelvic floor muscles have been held tightly for a long period of time, ie gymnastics, dancing, over-zealous Pilates. Continually drawing the abdominal muscles in can also contribute to overactive pelvic floor muscles. Being a generally ‘tight’ muscular person, ie lack of flexibility especially around the hip area.
Medical conditions Urinary tract infections or urination problems, yeast infections, sexually transmitted disease, endometriosis, genital or pelvic tumours, cysts, cancer, vulvodynia / vestibulodynia, pelvic inflammatory disease, lichen planus, lichen sclerosis, eczema, psoriasis, vaginal prolapse, etc
Childbirth Pain from normal or difficult vaginal deliveries and complications, c-sections, miscarriages, etc.
Age-related changes Menopause and hormonal changes, vaginal dryness / inadequate lubrication, vaginal atrophy
Temporary discomfort Temporary pain or discomfort resulting from insufficient foreplay or inadequate vaginal lubrication
Pelvic trauma Any type of pelvic surgery, difficult pelvic examinations, or other pelvic trauma
Abuse Physical attack, rape, sexual/physical abuse or assault
Medications Side-effects of some medications may cause pelvic pain
Examples of Non-physical Causes
Fears Fear or anticipation of intercourse pain, fear of not being completely physically healed following pelvic trauma, fear of tissue damage ie. ‘being torn’, fear of getting pregnant, concern that a pelvic medical problem may reoccur
Anxiety or stress General anxiety, performance pressures, previous unpleasant sexual experiences, negativity toward sex, guilt, emotional traumas, or other unhealthy sexual emotions
Partner issues Abuse, emotional detachment, fear of commitment, distrust, anxiety about being vulnerable, losing control
Traumatic events Past emotional/sexual abuse, witness of violence or abuse, repressed memories
Childhood experiences Overly rigid parenting, unbalanced religious teaching ie ’Sex is BAD’, exposure to shocking sexual imagery, inadequate sex education
No cause Sometimes there is no identifiable cause (physical or non-physical)
Source: https://vaginismus.com/vaginismus-causes/
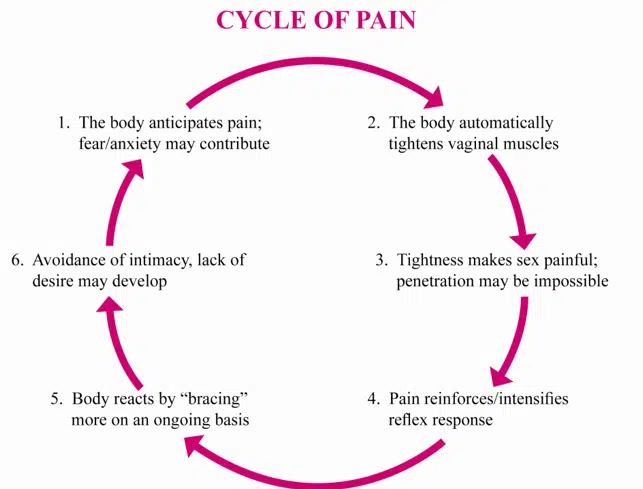
Vicious cycle of pain/tension
With vaginismus, when there is anticipation or fear of pain, or actual pain (eg. during intercourse or when trying to insert a tampon), the vaginal muscles tighten which makes penetration/insertion even more difficult, and further tensing can cause a cycle of pain.
How do the pelvic floor muscles contribute to vaginismus?
The pelvic floor muscles (PFM) play a key role in the function of a woman’s reproductive system, urinary tract, bowels and contributes to spinal stability. The muscles enable a woman to urinate, have intercourse, orgasm, complete bowel movements, deliver babies and they also support the spine and pelvis. An important group of muscles!
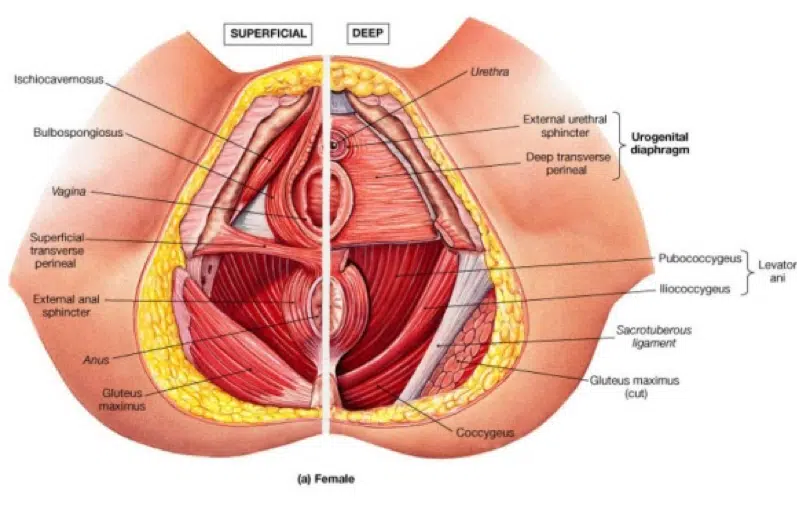
Some of the superficial and deep PFMs encircle the urinary opening, vagina, and anus in a figure-eight pattern with one loop of muscles surrounding the vaginal area and the other loop surrounding the anal area. On each end, the muscles are attached to the skeleton and support and hold in place the abdominal and pelvic organs like a net, forming the pelvic floor.
With vaginismus, the mind and body have developed a muscle memory or conditioned response against penetration. The body has learned to expect or anticipate pain upon penetration, so that the PFM ‘flinches’ or contracts to protect against the potential of intercourse pain. (A bit like automatically blinking one’s eyes and wincing when an object is hurled toward us). This is often a sub-conscious pattern and with vaginismus, you may not even realise that you do it or even know this is happening. Although acting as a defense mechanism against pain, the repeated tightening of the PFM ultimately causes pain. The overactive PFM may cause burning or pain upon penetration or movement and may even completely block entry. It may also result in pain after sex, difficulty with tampon use and/or changes in bladder behavior.
Frustration is common- women often know something is wrong but are unsure about what to do about it, which can lead to confusion and anxiety. But, keep in mind vaginismus is only tight PFMs and an amplified fear response. Muscles can absolutely be retrained to perform normally, and with the right approach, vaginismus can be completely resolved!
Painful Sex & Pelvic Physiotherapy
Have you ever had painful sex? Or are you afraid to get intimate with someone? Turn On interviewed physiotherapist Angela James from Sydney Pelvic Clinic about the psychological aspects of Genito-Pelvic Pain Disorder, also known as Vaginismus. Watch the two-part interview here:
What is the treatment for vaginismus? How can physiotherapy help?
Vaginismus is highly treatable as muscles are, by nature, very responsive. Pelvic floor physiotherapy, with a specially trained physiotherapist, will guide you through the appropriate steps to overcome vaginismus. A thorough subjective and objective assessment is imperative to guide an individual management plan for you. Your physiotherapist will ask questions, educate you about your anatomy, and will assess your pelvic floor muscles.
A fundamental part of the recovery from vaginismus is to find out where your pelvic floor muscles are, how to turn them on and more importantly, how to turn them off. This in conjunction with manual therapy (trigger point release, dilator therapy, pressure biofeedback) and a home management program is very effective in overcoming vaginismus.
After you have located and gained awareness of your PFM, the next step is to train them to respond differently to the anticipation of intercourse or tampon use. It is a learning process where you develop the skills necessary to take conscious control of this muscle group, and change the conditioned reflex so involuntary tightness no longer occurs. The ultimate aim is to regain control of your mind and body’s response to vaginal penetration, and allow you to enjoy comfortable sex.
The anticipation of pain, emotional anxieties, or unhealthy sexual messages can also contribute to and reinforce the symptoms of vaginismus. Frequently, but not always, there are underlying negative feelings of anxiety associated with vaginal penetration. Emotional triggers that result in or are a result of vaginismus are not always readily apparent and require some exploration. It is important that effective treatment addresses any emotional triggers, so a full pain-free and pleasurable sexual relationship can be enjoyed upon resolution. Please advise your physiotherapist if you require help with overcoming such emotional triggers.
Your physiotherapist will carefully monitor, guide and progress you through to complete recovery. If you have had pain or difficulty with intercourse or with tampon use, don’t suffer in silence! Please see your pelvic physiotherapist for an assessment so they can help you overcome your vaginismus.
References
Lahaie, MA, Boyer, SC, Amsel, R, Khalifé, S & Binik, YM (2010) Vaginismus: a review of the literature on the classification/diagnosis, etiology and treatment. Women’s Health, vol 6, no. 5, pp. 705–719
Melnik, T, Hawton, K, McGuire, H (2012) Interventions for vaginismus. Cochrane Database of Systematic Reviews, Issue 12. Art. No.: CD001760. DOI: 10.1002/14651858.CD001760.pub2.
This article was brought to you by:
Learn more about Angela James
Learn more about Alison Hui