How to best manage Gluteal Tendinopathy
Gluteal tendinopathy presents as pain and tenderness along the side of the hip, which may or may not refer down the lateral leg. Other terminologies used include: greater trochanteric bursitis, greater trochanteric pain syndrome (GTPS) or lateral hip pain. Epidemiology studies have found gluteal tendinopathy is more prevalent in females compared to males and is most common in middle age (Segal et al. 2007).
Gluteal tendinopathy is often described as a constant ache or bruise on the side of the hip, with pain at its worst in the morning. A diagnosis can be obtained from a physiotherapy assessment and confirmed on ultrasound or MRI scans. Scans will often show degenerative tears of the gluteus medius, gluteus minimus and or secondary bursitis, in conjunction tendinopathy (degeneration) of the gluteal tendon.
Activities that provoke lateral hip pain are often secondary to compressive forces on the gluteal tendon or sudden increases in tendon load. Compressive forces on the gluteal tendons occur when the hip is in an adducted position (when the hip crosses the mid line). In this position forces are increased on the iliotibial band (ITB) and the gluteal tendon is stretched and overloaded (Mellor et al. 2016). Provoking activities and postures that can lead to hip adduction include sleeping on the side (figure 2), walking upstairs, sitting with crossed legs (figure 7) and standing with a hitched hip (figure 3).
There are a number of anatomical, biomechanical and load related reasons as to why you might have developed lateral hip pain.
These could include:
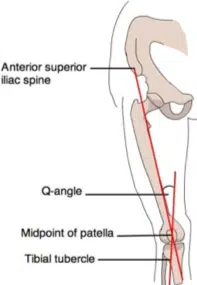
Having a wide hip angle (also known as a wide Q-angle)
- Q-angle refers to the natural angle of your hip. A line is drawn from the ASIS (bony prominence at the front of your pelvis) to the mid-point of the patella.
- Having a wide Q-angle increases compressive forces on the lateral hip, increasing the amount of time spent in hip adduction.
Biomechanics
- To maintain a neutral hip position while walking, climbing stairs and exercising adequate gluteal strength is required. Without adequate gluteal strength the hip will fall into an adducted position, causing increased gluteal tendon load and compression.
- Corrective exercises to strengthen the gluteals will off load the hip from compression and improve hip posture during exercise. Gluteals strengthening exercises have shown to have excellent long term outcomes in decreasing pain and increasing physical performance (Mellor et all 2018).
Load
- Sudden increases in load can also lead to gluteal tendinopathy. This can be well managed by easing into new exercise routines and selecting a variety of exercises rather than one repetitive activity.
To determine the reason behind why you have developed gluteal tendinopathy you will require an individualized physiotherapy assessment. A thorough physiotherapy assessment ensures that all contributing factors are addressed and your rehabilitation is targeted to the root cause of your problem. It is also important to note there are other causes of lateral hip pain, such as referred pain from the lower back, and it is important this is ruled out before commencing treatment.
There are some simple strategies to reduce compressive forces on the gluteal tendon, and below are some tips to avoid further exacerbation of symptoms. Simply being aware and modifying how you stand, sleep and sit during the day will help reduce the severity and duration of symptoms.
Tendon care tips
1. Standing posture
Stand in a neutral hip position and avoid hip hitching (where you push or drop one hip out to the side). To reduce compression on the glute tendon and ITB, stand with feet hip distance apart, evenly distribute your weight between both feet and maintain a neutral pelvic position.
1. Standing posture
Stand in a neutral hip position and avoid hip hitching (where you push or drop one hip out to the side). To reduce compression on the glute tendon and ITB, stand with feet hip distance apart, evenly distribute your weight between both feet and maintain a neutral pelvic position.


2. Sleeping position
Lying on your side can compress either the top or bottom gluteal tendons. If your lateral hip pain is severe, you may need to avoid sleeping on that side for a few weeks. To avoid compression in the top hip, place a firm thick pillow between your knees to keep your knee in line with your hip.


3. Sitting positions
Be aware of how you’re sitting during the day, do you sit with your legs crossed? Sitting with one leg crossed over the other, puts both hips into an adducted position increasing compression on the gluteal tendons. Aim to sit with the knees at hip distance and feet resting on the floor.


4. Stay active
Keep exercising! Gluteal tendinopathies are more than often degenerative in nature and require ongoing load. If you find you get worse with more rest, it’s a good sign you need to keep up with your usual exercise routine to keep the tendon happy. Degenerative tendons usually get worse with rest, so sitting around and waiting for it to “heal” usually won’t help.

Remember it is the accumulation of hip adduction that will provoke gluteal tendinopathy, so try not to worry if you find yourself in a poor standing or sitting position every now and then. For long-term management progressive gluteal strengthening will off load the hip and has been shown to have excellent outcomes in decreasing pain and physical performance (Mellor et all 2018).
FAQ’s about lateral hip pain
My hip hurts when I sleep on it, what can I do?
Pain during side lying is a common feature of gluteal tendinopathy refer to tip 2 “sleeping position” to best set up your sleeping position. If you can, try sleeping on your back.
My hip hurts when I wake up in the morning..
Morning pain is a hallmark symptom of gluteal tendinopathy, even if you slept in a good position. Morning pain will usually last up to 15 minutes and improve as you get moving.
My doctor says I have hip bursitis..
You can have greater trochanteric bursitis in conjunction with gluteal tendinopathy, but bursitis itself is not an isolated pathology. The bursa is a fluid filled sac that sits underneath the gluteal tendon and can become compressed and irritated. Management strategies are similar to lateral hip pain, but we might try a few different things too so it’s best to have a physiotherapy assessment to make a management plan.
Do I need a corticosteroid injection?
A cortisone injection into the lateral hip can be indicated if symptoms are extremely inflammatory in nature. However as this injection is a steroid, it can ultimately lead to tissue degeneration and further tendon disorganization. To avoid potential risks and complications of the injection, it is recommended to trial a period of conservative therapy with a physiotherapist first.
Should I keep exercising? Or do I need to rest?
Refer to tip 4, keep moving! Most gluteal tendons are degenerative in nature and you need to keep exercising to maintain the tendons tolerance to load. Too much rest often leads to deconditioning and muscle loss.
Are there specific exercises I need to do?
Yes, progressive strength exercises are required to assist in reducing pain, increasing muscle strength and improving physical function and performance. The correct exercises will be selected by a physiotherapist, based on why you have developed lateral hip pain in the first place.
Contributor
Cherie Redfern-Hardisty
Physiotherapist
References
Mellor R, Grimaldi A, Wajswelner H, et al. Exercise and load modi cation versus corticosteroid injection versus ‘wait and see’ for persistent gluteus medius/minimus tendinopathy (the LEAP trial): a protocol for a randomised clinical trial. BMC Musculoskelet Disord 2016;17:196. doi:10.1186/s12891-016-1043-6
Mellor R, Bennell K, Grimaldi A, et al. Education plus exercises versus CSI use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. BJSM 2-18; 361.
Segal NA, Felson DT, Torner JC, et al, Multicenter Osteoarthritis Study Group. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil 2007;88:988-92. doi:10.1016/j.apmr.2007.04.014