
Hip Impingement
Here at Sydney Pelvic Clinic we often see patients presenting with hip pain and one of the most common causes is hip impingement. Research tells us that 87% of patients presenting with hip pain fit the diagnostic criteria for hip impingement, also known as femoroacetabular impingement, abbreviated as ‘FAI’ (Ochoa et al., 2010).
In this article, we will share with you all that you need to know about FAI, including:
- Etiology (what causes hip impingement)
- Signs and symptoms
- How is it diagnosed
- How physiotherapy can help
- When a specialist review is indicated
So if you suffer from hip pain or know any one that does, this is the article for you!
What Causes FAI (hip impingement)?
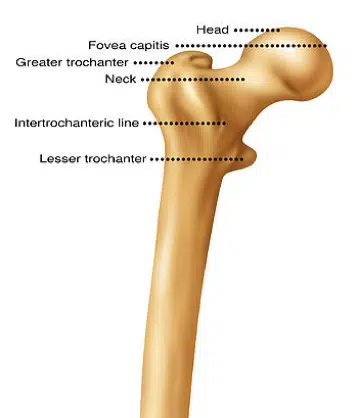
First let’s discuss the normal boney anatomy of the hip joint. The hip is a ball and socket joint. The pelvis houses the circular concave ‘socket’ part of the joint, known as the acetabulum, and the top of the thighbone forms the circular convex ‘ball’ part of the joint, known as the femoral head.
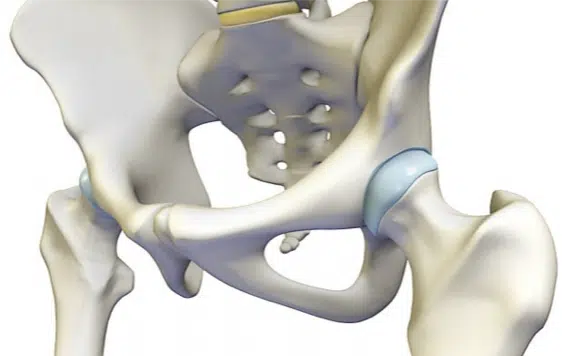
This circular femoral head morphs into a skinnier concave femoral neck. In an ideal world these boney ends are perfectly shaped to create a joint that is both stable yet mobile, allowing us good functionality of our hips.
The shape of your hip joint should be such that it allows you to bend your hips deeply into a low squat, or extend to create long and meaningful strides, move side to side and rotate to allow you to step out of the car, or provides you with multi-directional agility to maneuver and out-run your opponent. Whether you are an elite sports player or an avid gardener, we all need good hip range to live life to the full.
Hip impingement occurs when there is abnormal boney contact between the two parts of the joint, e.g. the acetabulum makes contact with the femur when the hip is ‘flexed’ or bent. Some examples of when the hip is bent include a deep squat, sitting, cycling, getting out of a car, breaststroke with a frog kick, or moving side to side in a football scrum.
Hip FAI occurs for two main reasons:
1. Changes to the boney anatomy of the hip joint
Research shows that 20% of the general population and 60-90% of the athletic population have variations in the boney shape of their hip joints (Frank et al., 2015). These changes can be a deeper hip socket, known as a pincer deformity, and/or a thicker, bumpy femoral neck, known as a Cam deformity. When these boney changes are combined with poor muscular control this can result in hip impingement, and lead to discomfort.
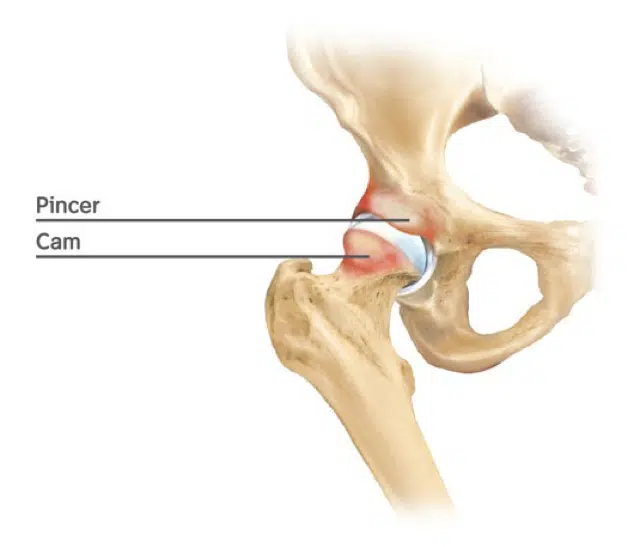
The athletic population have a high incidence of Cam and Pincer deformities due to the increased load that is placed on the hip throughout development. During an adolescent growth spurt, if a continual load is present, such as a high volume of sporting activity, there will be increased boney lay-down, resulting in Cam and/or pincer deformity.
2. Dysfunction of the muscles around the hip
Despite the presence of a pincer or cam deformity, hip impingement is less likely tooccur if the muscles around the hip are functioning well. If the muscles as high as the core and as low as the foot and ankle are strong the hip is less likely to impinge with provocative tasks such as deep squats, running, jumping, sitting etc. This would explain why only half of the athletic population with a Cam or Pincer deformity have a history of hip pain. In the general population only 23% with a Cam or Pincer deformity have a history of hip pain (Frank et al., 2015).
So what is the difference between those that do and don’t have pain?
The answer is the MUSCLES!
If the muscles around the hip are weak this can result in poor hip control and alignment, with the resultant effect of hip impingement and pain (Yépez et al., 2017).
Here are some examples of good hip alignment versus poor hip alignment:

Example 1
Correct squat technique with good hip alignment

Example 2
Poor squat technique with poor hip alignment which can lead to impingement
Example 3
Correct single leg squat technique with good hip alignment
Example 4
Poor single leg squat alignment which can lead to hip impingement
Quick Quiz: what is your hip alignment like when you squat? Take a moment to check this in the mirror.
What are the common signs and symptoms of FAI (hip impingement)?
Hip pain (at rest or with activity) in any of the following locations:
- Front of the hip around the upper thigh
- Groin
- Back or side of the hip around the gluteal area
Also:
- Pain with prolonged sitting
- Pain with a deep squat position
- Pain with hugging knee to chest
- Stiffness in the hip joint
- Catching/clicking in the hip joint
- Reduced ability to participate in sporting activities and activities of daily living
Diagnosis
Diagnosis is generally quite easy and simple and in most cases only requires a physiotherapy assessment. During this assessment we perform different hip tests, including one specific hip test called the FADIR test (anterior impingement test) which is more than 90% accurate in detecting FAI (Thomas et al., 2013). Other important assessments include:
- Analyzing posture and movement patterns, including walking, squatting and balance
- A detailed assessment of hip joint range
- Specific hip tests, including the FADIR test previously mentioned
- Muscle strength assessment
Muscle Strength Assessment
The assessment will include a hip strength screen using a hand-held dynamometer, which is a small device with a force plate. This device allows us to measure the strength of the muscles around the hip and pelvis. We can assess for symmetry and balance in the body. We know from research that the hip muscles should be symmetrical, i.e. the left hip muscles should be as strong as the right, and that certain muscle groups should be stronger than others.
For instance, particular gluteal muscles should be stronger than the hip flexor and groin muscles (Kemp et al., 2012). If the gluteals are weak this can lead to poor hip alignment as previously shown in the images above. The physiotherapy assessment can decipher the need for imaging, such as a plain hip x-ray, or an MRI with contrast.
Finally, How Physiotherapy Can Help!
Once a thorough physiotherapy assessment is completed, a specific and individualised treatment plan can be developed. This treatment plan is centered on the patient’s goals and the activities they would like to participate in. A treatment plan can involve any of the following:
- Advice on pain relief
- Advice on activity modification
- Manual therapy to reduce muscular tension, restore range of motion and reduce hip pain; including massage, myofascial release, dry needling and/or cupping
- Specific stretches to restore hip range of motion
- Tailored exercise rehabilitation to address any muscle weakness detected during the assessment. Rehabilitation is not limited to the muscles around the hip but addresses the body as a whole
Physiotherapy varies greatly between individuals, as no one hip is the same. The period of time to rehabilitate the hip also varies, but generally takes 2-6 weeks to see an improvement in hip pain and a minimum of 6-12 weeks to see improvement in muscle strength.
In our clinic, we work closely with your medical team, such as your GP, orthopedic surgeon and sports physician, we refer on if an improvement is not seen within 6 weeks of treatment.
Let’s wrap up with the knowledge that hip pain is 100% treatable! So if you, or any of your friends or family suffer from hip pain, come and see one of our friendly pelvic physiotherapists and get started on the road to a more mobile, strong and pain-free hip.
References
FRANK, J. M., HARRIS, J. D., ERICKSON, B. J., SLIKKER, W., 3RD, BUSH-JOSEPH, C. A., SALATA, M. J. & NHO, S. J. 2015. Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthroscopy,31, 1199-204.
OCHOA, L. M., DAWSON, L., PATZKOWSKI, J. C. & HSU, J. R. 2010. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clinical orthopaedics and related research,468, 2710-2714.
YÉPEZ, A. K., ABREU, M., GERMANI, B. & GALIA, C. R. 2017. Prevalence of femoroacetabular impingement morphology in asymptomatic youth soccer players: magnetic resonance imaging study with clinical correlation. Revista brasileira de ortopedia,52, 14-20.
Thomas, G. E., Palmer, A. J., Andrade, A. J., Pollard, T. C., Fary, C., Singh, P. J., … Glyn-Jones, S. (2013). Diagnosis and management of femoroacetabular impingement. The British journal of general practice : the journal of the Royal College of General Practitioners, 63(612), e513–e515. doi:10.3399/bjgp13X669392
