We are often told we need to squeeze and tighten the pelvic floor muscles but in some cases this can be the wrong advice. This month we will discuss overactive pelvic floor muscles (PFM), which can lead to pelvic pain. Did you know that pelvic pain affects 1 in 5 women (Fall et al, 2010) and 1 in 12 (Ferris et al, 2010) men? That’s as common as shoulder pain!
What are overactive pelvic floor muscles?
PFM overactivity is a condition where there may be increased PFM tension at rest, increased voluntary or involuntary contractile activity, or a decreased ability to fully relax the PFMs.
What are Hypertonic Pelvic Floor Muscles?
Sometimes overactive pelvic floor muscles are also known as hypertonic pelvic floor muscles.
What causes overactive PFMs?
There can be many different contributing factors:
- Trauma- eg. a fall onto the buttocks/tail bone which causes the PFMs to tighten protectively, or trauma like sexual abuse
- Injury – PFMs can also tighten as a compensation strategy, for example, following a hip, knee or ankle injury/surgery that was never fully rehabilitated
- Infection or inflammation – eg. chronic urinary tract infections or chronic thrush
- Pelvic surgery- this can cause scar tissue or irritate pelvic structures including ligaments, nerves and muscles, eg. post-hysterectomy or post-prostatectomy pain
- Chronic holding patterns – some people will constantly grip through their abdominals, PFMs and/or buttocks as learnt behaviours and postures
- Hypermobility – some people with excessive hip and pelvic mobility can compensate through PFM tightness
- Stress- tension can be stored in the PFMs in response to stress. Think of the image of a dog who is frightened with its tail tucked under… that is due to the PFMs pulling!
- Bladder or bowel dysfunction- if there is a frequent sensation of urgency or chronic constipation, the PFMs often have to work hard to hold the bladder or bowel motions in
What are the signs and symptoms of having overactive PFMs?
Some possible signs and symptoms include:
In men:
- Not being able to feel a PFM contraction or release
- Pain in the penis, testicles and/or rectum
- Urinary urgency or frequency
- Slower urinary flow or the feeling of incomplete emptying
- Difficulty or pain with emptying the bowels or passing ‘skinny stools’
- Erectile dysfunction
- Premature ejaculation
In women:
- Not being able to feel a PFM contraction or release
- Pelvic pain that can include urethral, vaginal, rectal, lower abdominal pain
- Urinary urgency or frequency
- Slower urinary flow or the feeling of incomplete emptying
- Inability to have sex or pain with sex, either with initial or deep penetration
- Difficulty or pain with emptying the bowels or passing ‘skinny stools’
- Stress urinary leakage in some cases
What does treatment for overactive PFMs involve? What can physiotherapy do?
It is essential to teach the PFMs how to relax fully first before being able to gain full range and strengthen all the muscle fibres. This is a condition where squeezing and tightening the PFMs too soon could make things tighter!
To help your PFMs let go, treatment can include:
- Belly breathing and relaxation techniques
- Education and biofeedback (eg. real-time ultrasound)
- Manual therapy techniques including external and internal (ie. vaginal and/or rectal) myofascial techniques
- Work on calming the sympathetic nervous system, eg. mindfulness, yoga
- Therawand for self-release
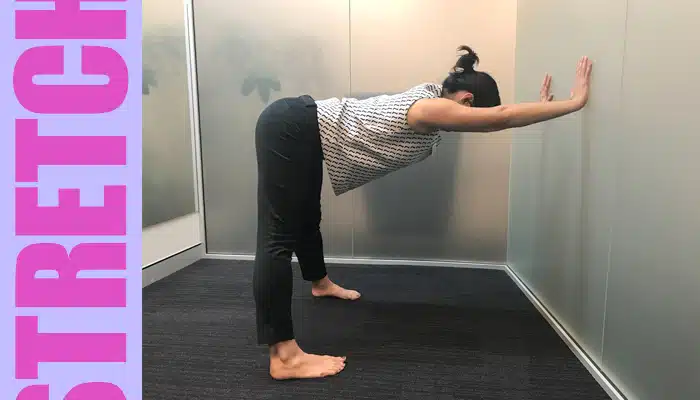
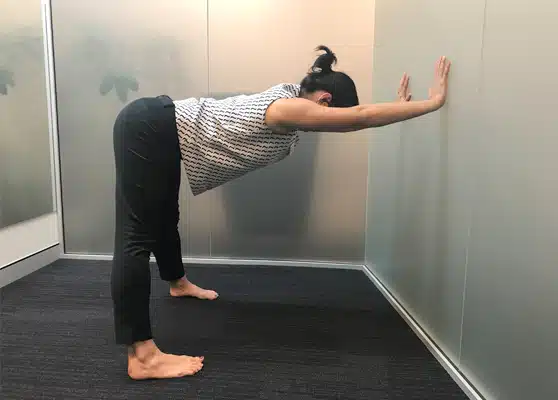
- Stretches (See the table stretch below)
- Sometimes strengthening gluteal muscles is indicated to offload the PFMs
I think I might have overactive PFMs – what should I do?
Come and see a Sydney Pelvic Clinic physiotherapist who will be able to examine you to check. For the most accurate assessment, this will involve a vaginal and/or rectal examination for women, or a rectal examination for men. Your physiotherapist will then be able to determine whether your PFMs are indeed overactive and if you should avoid over-squeezing or tightening. We will help find the right plan for you to regain optimal pelvic health.
Watch Ange in the short video below talk about mindful PFM connection and release:
This article was brought to you by:
Learn more about Alison Hui