In Australia, pelvic pain affects 1 in 5 women and 1 in 12 men every year: it’s as common as shoulder and neck pain! Despite this prevalence, a pelvic pain condition called Pudendal Neuralgia (PN) flies well under the radar, even though its impact on sufferers can be devastating. PN is a painful, uncomfortable pelvic condition which affects bladder, bowel and sexual function in both men and women. The good news is that PN is treatable, but the lack of information about the condition, coupled with the embarrassing location of the symptoms, often leads to delays in diagnosis and unnecessary surgical or medical intervention. Sydney Pelvic Clinic is passionate about increasing community awareness of PN and helping patients to commence early, effective and appropriate management for this condition.
What is Pudendal Neuralgia?
PN is pain or an altered sensation anywhere along the pudendal nerve pathway, which is from the sacrum to the pubic bone (see the diagram below). The pudendal nerve starts at your sacrum (S2-4), travels towards the sacral spine, through the Alcock’s canal and then runs along the pubic bone.
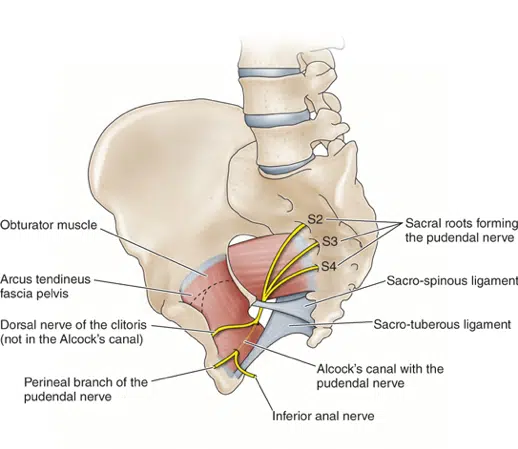
Three branches of the pudendal nerve supply the rectum, perineum and clitoral/penis regions. The pudendal nerve travels alongside key pelvic muscles and is made up of sensory, motor and automatic nerve fibres. Due to the complexity of this neural network, symptoms of PN can range widely.
What are the Symptoms of PN?
PN symptoms may include pain, altered sensations and changes in stress and anxiety levels. PN pain is often described as being sharp, burning or stabbing, or it can feel like a prickling, itching or a swollen sensation in the rectum or perineum. Patients describe a hot poker-like sensation or they say they feel like they have a constant bladder infection, even though test results are clear. PN is often worse when you are sitting, especially on a hard surface. Many patients find the pain is reduced if they sit on a cushion or by standing up.
How do you get PN?
PN occurs when the pudendal nerve fibres are irritated or compressed. Think of when a garden hose is kinked: the water flow is reduced. This nerve compression can be a result of tension in the pelvic muscles, or from excessive sitting on hard surfaces that compress the inside of the SIT bones; for example, sitting on a bike seat where the SIT bones are wider the seat. The pudendal nerve can also be irritated from over-stretching in vaginal delivery, when it can stretch up to 3 times beyond its usual length. Surgery such as hysterectomies or hip surgery may also affect the nerve. In a condition called Pudendal Nerve Entrapment (PNE), the nerve becomes trapped. PNE is much less common than PN, and may require a surgical resolution.
How is it Diagnosed?
The diagnosis of PN is largely based on clinical findings (Nantes criteria, Labat et al 2008). Rarely are scans, investigations or blood tests needed to reach a diagnosis of PN. At times, a pudendal nerve block may be useful if the clinical tests are unclear.
What is the Treatment for PN?
Pelvic Physiotherapy is first line management for patients with PN. You should be given an individual plan tailored to your needs, which may include:
- Education and reassurance
- Specific internal and/or pelvic myofascial release to reduce the irritation/compression of the muscles onto the pudendal nerve
- This could involve vaginal or rectal treatment to access the deeper muscles in the pelvis
- Pelvic stretches or pelvic nerve glide exercises
- Medication may be useful to calm down the nervous system
- Lifestyle advice
- Appropriate exercise rehabilitation
Can I Recover from PN?
Yes. With an early diagnosis, and the right management plan in place, patients can expect to make a full recovery from PN. The body has an enormous potential for change, and is always seeking balance. Pelvic Physiotherapy can help you restore balance in the pelvis, so you can get back to normal life without the burden of PN.

