If you’ve been experiencing vulva pain, it could be an indication of a wide number of conditions. There are many female sexual pain conditions that can lead to pelvic pain, vulva pain, or vaginal pain, greatly impacting a woman’s quality of life.
Vulvodynia is one of those conditions, characterized by vulva pain that lasts longer than three months. If you’ve been experiencing persistent vulva pain, it could be this condition affecting you.
This condition can be painful to deal with, but those with it are not alone. In fact, it’s estimated that 8 per cent of Australian women 18-64 have reported chronic pain in their vulva during their lifetime. A firm understanding of vulvodynia, and how it impacts women, can help women better deal with vulvodynia and its impact.
Let’s take a look at what defines vulvodynia, its conditions, and how it can impact a woman’s quality of life.
What is Vulvodynia?
Vulvodynia is a chronic vulvar pain condition that presents itself seemingly without cause. Like other chronic pain conditions, vulvodynia symptoms and how they present will vary from person to person. Those with generalized vulvodynia will feel pain around the entire vulva area. Those with localized vulvodynia will only feel vulva pain in a certain area, likely the vagina opening.
The most common symptom is the presence of consistent chronic pain that lasts longer than three months. This pain is often described as a burning/sore sensation. Other symptoms include stinging, throbbing, and itching at the vaginal opening.
Painful sexual intercourse is another symptom, and often the way women find out they are dealing with chronic vulva pain. Those suffering from vulvodynia pain often find it difficult to do anything internally, whether it be tampon insertion, a pelvic exam, or sexual intercourse, because of the pain.
What Causes Vulvodynia?
Unfortunately, vulvodynia is a chronic vulvar pain condition that, unlike other forms of female sexual pain, has no identifiable cause. There are no infections, diseases, or viruses that cause this condition to appear.
The positive is this condition cannot be “caught” meaning there’s no concern about giving it to a partner. However, it also means dealing with the frustration of not knowing where the pain has come from.
Current research theorises that vulval pain from vulvodynia could be caused by an injury to nerves around the vulva, an increase in the number of vulva nerves, changes to pelvic floor muscles, or even genetic susceptibility to the condition. However, none of these are known for sure.
How is Vulvodynia Treated?
Treatment for vulvodynia varies from patient to patient, with the goal being to alleviate pain. Typically, treatment will start with a combination of treatments, including Physiotherapy and prescribed medication.
A great first step is to make an appointment with a pelvic Physiotherapist who is qualified in working with pelvic muscles, for pelvic floor therapy and specific exercises that can help alleviate or manage pain. To manage pain, many women will be prescribed pain-blocking medications to lessen chronic pelvic pain. As this condition can greatly impact a person’s mental state, healthcare professionals will pair treatments with visits to a psychologist as a treatment option, to help the patient’s mental health.
While these treatments are no guarantee that the pain will disappear, with the right routine, many women do find that their pain symptoms can be greatly relieved.
How Does Vulvodynia Affect Your Quality of Life?
Vulvodynia can impact women in a number of ways:
The Cycle of Pain
Dealing with chronic pain is a complex, physiological process. Those with vulvodynia are living in a body where their brain is constantly receiving pain signals. Normally, the body will send pain signals to help your body know what to heal, turning them off once the injury is gone.
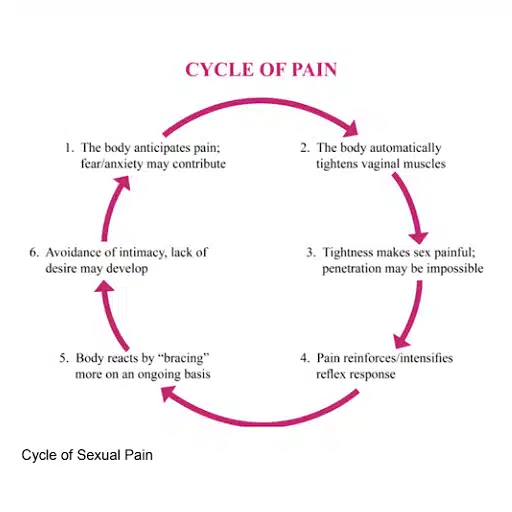
With chronic pain, the signals never shut off, whether or not your body has “healed.” This pain can last months, years, or even a lifetime, depending on the condition. Eventually, the mental impact of chronic pain can lead to the “cycle of pain” which can make the pain even worse. The cycle works as follows:
This cycle can be hard to break given the heavy impact pain has on mental health and our thought processes. That’s why it’s important to find support for the mental impact chronic pain can have. Reach out to family and friends or seek out professional mental health support.
Vulvodynia and Sex
The largest impact of this condition, for many women, is the way it impacts their sex life and intimate relationships. Experiencing chronic pain in the genital area is a huge hurdle to participating in sexual activity. An inability to participate can make many women depressed and worried about the negative impact the condition has on their intimate relationships.
The important thing to remember is that you are not alone, and you can still have a wonderful sex life even if it’s free of sexual intercourse. If you are struggling with vulvodynia and sex, try the following:
Communicate
Communication is key when it comes to sex, even more so when one person is experiencing chronic pain. It’s important to make sure your partner knows what you feel, and not just physically.
If vulvodynia is impacting your sex life, talk with your partner about it. Explain your condition to your partner and create a space for open dialogue between the two of you. Discuss how vulvodynia has impacted your approach to sex and allow your partner to do the same. Try to really listen to one another and let each partner express their experience.
Explore Different Types of Sex
With a deeper understanding of how this condition has impacted your approach to sex, you can then take steps to explore new forms of intimacy. For many couples, sex can be defined by the act of intercourse. But luckily, there are different things you and your partner can do that don’t require it.
Talk with your partner about what hurts, but also discuss the things that do feel good. You can focus on non-penetrative sex acts and intimacy and try something new.
Seek Support
This condition can be painful physically, and emotionally. If you and your partner are struggling to talk about this condition, there’s no shame in reaching out to help. A sex therapist can be a great third party to help you and your partner work through your feelings around sex, intimacy, and dealing with chronic pain.

