With Sydney Pelvic Clinic’s Alison Hui, APAM.
Prostatitis-related conditions are the most commonly diagnosed urological issue in men under the age of 50, manifesting in symptoms such as pelvic pain, bladder and sexual dysfunction, and psychological issues. Sometimes prostatitis is due to a bacterial infection, however, 90-95% of cases are considered non-bacterial and fall under the Chronic Pelvic Pain Syndrome (CPPS) category (Doiron, Shoskes & Nickel, 2019). As such, many of our patients have often been to the doctors and returned negative tests for urinary infections or sexually-transmitted infections, their ultrasounds appear normal, and antibiotics have not helped to improve their symptoms.
CPPS is the occurrence of persistent pelvic pain where there is no proven infection or obvious pathology to account for the pain, and it can affect 8-11.5% of men (Clemens et al, 2019).

Causes
The triggers of male pelvic pain/ CPPS are many and varied but may include:
- Infection- such as a urinary tract infection or sexually transmitted infection which can trigger the initial onset of pain. Pain can persist, however, even after the infection has resolved
- Trauma – like a fall onto the tailbone or soft tissue injuries from sports or sexual activity
- A history of physical, sexual or emotional abuse
- Stress and/or anxiety
- Change/ increase in exercise intensity
- Prolonged sitting
- Low back/hip pain and tight muscles
The factors above can lead to inflammation, pelvic floor muscle tension and sensitisation of the body’s nervous system, which can lead to persistent pelvic pain and symptoms.
The Symptoms of CPPS May Include:
- Pain in the urethra, penis, testicles, scrotum, perineum, rectum or suprapubic region – pain can be aggravated by urination, ejaculation and/or having a bowel motion, stress or sitting
- Bladder symptoms such as urinary frequency and urgency; urge urinary incontinence; slower or stop-start urinary flow; post-void dribble
- Sensation of incomplete bladder or bowel emptying
- Sexual dysfunction – erectile dysfunction; premature ejaculation; pain on ejaculation
How can Physiotherapy Help with CPPS?
Physiotherapy is a crucial part of multi-modal treatment of CPPS (Doiron, Shoskes & Nickel, 2019).
Your pelvic Physiotherapist will take a detailed history of your condition (including questions about bladder, bowel and sexual function) and other medical issues, while considering any social and emotional factors that could be contributing to your symptoms. A thorough physical examination would generally include an assessment of your breathing mechanics, biomechanics that could be contributing to muscle imbalance, and an assessment of the pelvic floor muscles (PFM) via real-time ultrasound and/or a rectal examination to check for any increase in tone or tenderness. Most men with CPPS (up to 88%) have tenderness in their PFM and poor pelvic floor function (Zermann et al, 1999).
Physiotherapy Management of CPPS Should be Holistic in Nature, Using a Biopsychosocial approach, and Should Include:
- Pelvic floor muscle down-training /re-training/ biofeedback
- Breathing and relaxation techniques
- Pain science education
- Lifestyle advice and strategies to help calm the nervous system
- Manual therapy to external and internal pelvic muscles as required
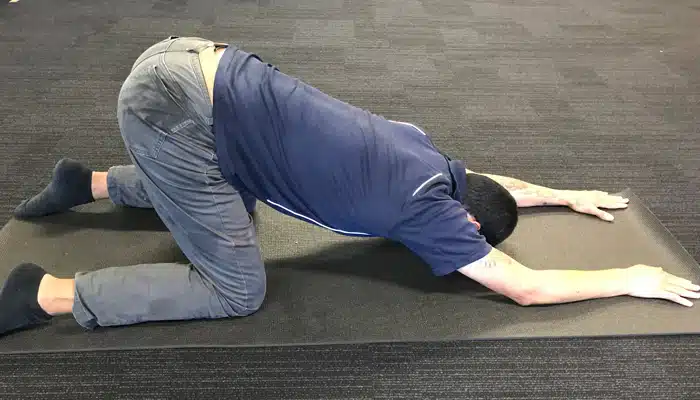
- Stretches and home exercises
- Building a personalised self-management program to help you better manage your symptoms
- Multidisciplinary approach and collaboration with other service providers– eg. GP; urologist; pain specialist; psychologist; personal trainers
Two Useful Positions

If you have been struggling with male pelvic pain/ CPPS, please book in to see one of our pelvic Physiotherapists who can assess, diagnose and provide expert individualised management to help you regain optimal pelvic health.
References
Clemens JQ, Mullins C, Ackerman AL, Bavendam T, van Bokhoven A, Ellingson BM, Harte SE, Kutch JJ, Lai HH, Martucci KT, Moldwin R, Naliboff BD, Pontari MA, Sutcliffe S, Landis JR; MAPP Research Network Study Group. Urologic chronic pelvic pain syndrome: insights from the MAPP Research Network. Nat Rev Urol. 2019 Mar;16(3):187-200.
Doiron RC, Shoskes DA & Nickel JC. Male CP/CPPS: where do we stand? World Journal of Urology (2019) 37:1015–1022
Zermann DH, Ishigooka M, Doggweiler R, Schmidt RA. Neurourological insights into the etiology of genitourinary pain in men. J Urol 1999; 161:903.

