What is Osteoporosis?
Osteoporosis (OP) is a condition of low bone mineral density (BMD). It causes fragile and brittle bones where fractures are more prevalent. The most commonly affected areas are the spine, hip, upper arm, wrist, ribs or forearm.
Epidemiology data reports 70% of people in NSW & ACT aged 50 years and older have osteoporosis or osteopenia; this is 1.9 million people (Sanders et al. 2017). Year on year prevalence continues to rise with the ageing population. Women are more likely to suffer from OP, specifically after menopause, as bone loss is higher as estrogen levels decrease.
Other risk factors include:
- Family history of OP
- Low calcium and vitamin D levels
- Medical history: use of corticosteroids, hormone levels and thyroid conditions
- Low levels of physical activity
- Smoking
- Excessive alcohol intake
If you are over 50 and have suffered a fracture after a minor incident, it is important you are investigated for osteoporosis as it is a “silent disease” and you may not have any other signs or symptoms.
How is Osteoporosis Diagnosed?
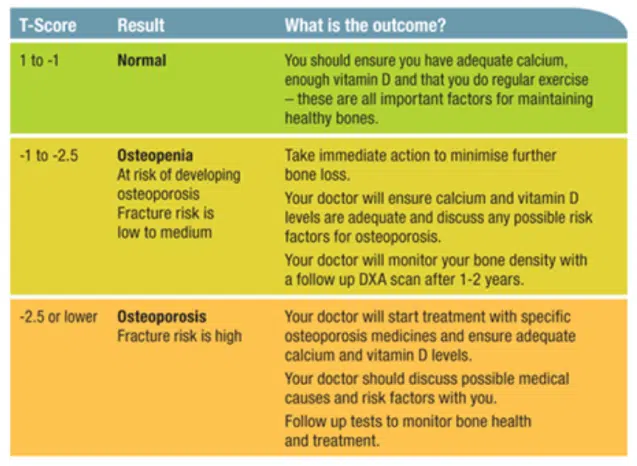
If your care team suspects low bone mineral density, a GP will refer for a DEXA scan. A DEXA scan is the most specific way to determine bone mineral density, a T-Score is then calculated to make a diagnosis. A DEXA scan includes BMD readings in the wrist, hip and lumbar spine. According to the World Health Organisation (WHO) the following scores determine osteoporosis severity.
- A T-score of -1.0 or above is normal bone density
- A T-score between -1.0 and -2.5 means low bone density or osteopenia
- A T-score of -2.5 or below is a diagnosis of osteoporosis
I Have Been Diagnosed with Osteopenia or Osteoporosis, What Should I Do?
Osteoporosis severity will determine what happens next (refer to image 1 below). A GP usually manages mild-moderate BMD loss and they may refer you to an Endocrinologist for further medical management if indicated.
Pharmacological interventions may be prescribed to assist in rapid bone rebuilding. Calcium and vitamin D levels should also be checked as adequate levels are crucial to maintain and build bone. Exercise is the only other way to increase or stimulate bone growth. After a diagnosis of OP it is absolutely necessary to either commence or modify exercise to ensure its’ impact is as effective as possible.
Exercise for Osteopenia and Osteoporosis
Exercise is the most effective lifestyle strategy to maintain healthy bones, it can assist in building and maintaining bone density. Specific loading through strength training has also been shown to be an effective way to treat osteoporosis (Liftmor 2019).
What Kind of Exercise is Best to Build Bone?
Exercise at difference ages has different impacts. Adults need a combination of progressive resistance training and moderate impact weight-bearing activities. These specific types of exercise will increase BMD and prevent further bone loss. The key here is exercise TYPE and progressive increases in resistance.
Optimal exercise guidelines
- Regular: at least 3 x per week
- Challenging: heavier weights with fewer repetitions
- Progressive: exercise difficulty needs to increase over time
- Varied: routines need to have variety, bone adapts to exercise and stops changing if you continue the same set of exercises
- Short intensive bursts of weight bearing exercise are more effective than slow movements
What Type of Exercise Should I be Doing?
- Highly osteogenic (best for building bone):
- Jumping
- Impact aerobics
- Progressive resistance training
- Dancing
- Sports e.g. Basketball or netball
- Moderately osteogenic (some ability to build BMD)
- Running or jogging
- Brisk walking or hill walking
- Stair climbing
- Low osteogenic effect (minimal effect on bone mineral growth)
- Leisurely walking
- Lawn bowls
- Yoga or Pilates
- Tai Chi
- Non-osteogenic (no effect on bone mineral growth)
- Swimming
- Cycling
It is most effective to do three activities per week, aiming for activities that are HIGHLY OSTEOGENIC.
Are There any Types of Exercise I Cannot do with Osteoporosis? Do I Need to be Careful?
There is no specific exercise that is completely off-limits. In fact, recent research has found that high-intensity and impact training, previously thought to be high fracture risk, to be safe in the osteoporotic population (LIFTMOR Trial, 2019). This research also found this type of exercise to enhance bone strength when compared to lower intensity type exercise.
However, for those with either osteoporotic spinal fractures, or a history of such fractures, it is worth considering end of range spinal positions, including: flexion, extension and rotation of the spine. End range spinal positions theoretically increase vertebral body load, thought to increase risk of a wedge or compression fracture. This is definitely not to say you can’t bend forward/backward or rotate to the side, but if loads are excessive or repetitive, the load has the potential to cause injury. This is why exercise programs need to be specific to each individual and exercise programs need to be monitored.
Exercise intensity, selection, variety and the overall program should be matched to capabilities and training history. Muscle strength and endurance in the tissue surrounding your bones will greatly influence your overall exercise capacity, as will current and previous exercise history. Exercise programs should be developed by either a Physiotherapist or exercise physiologist, who are trained in exercise therapy in chronic disease. This will help to ensure optimal outcomes while avoiding potential pain flare-ups or overload.
For exercise to have the biggest possible impact you need to participate in regular exercise (at least 3 x per week), choose exercise/activity that has high or moderate osteogenic (bone building) effects and change your schedule regularly.
Exercises to Get You Started
The femoral neck and the spine are two high-risk areas to suffer osteoporotic fractures. Targeted strength training in muscles surrounding these joints aims to directly increase BMD and surrounding muscle bulk. The following are examples of exercises that target these areas.
*As this information is a general guide only, the following exercises do not take into consideration other pathologies or injuries. This does not substitute for a Physiotherapy exercise plan.
Sit to Stand

- Start sitting on a chair, feet hip width apart
- Arms out in front
- Rise from the chair by shifting body weight forward into the heels of the feet
- Stand with control, completely straighten hips and knees at the top
- Lower with control to sitting
To make easier: start with bottom further forward in the chair or use a higher chair.
To make more difficult: hold arm weights, use a very low chair or hold each phase as pictured for 5 seconds.
Step-Ups

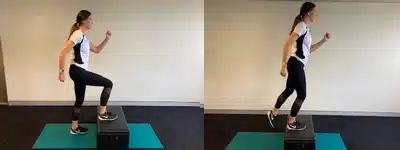
- Keeping feet hip distance, place one foot on the step
- Push up onto the step, and straighten your hip and knee with control
- Place opposite foot up on the step
- Descend with control
To make easier: use a lower step or hold on to the wall for balance.
To make more difficult: use a higher step (picture b), hold hand weights, or add a single leg jump at the top (this requires balance, strength and coordination).
Deadlifts

- Start with feet hip width apart, knees behind toes, in a low squat position
- Keeping arms straight holding weights
- Drive up to standing by straightening your back and hips
- Keep weights close to you
- Lift and lower with control, descend as far as your hips and back are comfortable
To make easier: use light weight, move through a small range of motion.
To make more difficult: heavier weights, increase speed and depth of the motion.
Active Prone Extensions

- Lie face down on a firm surface, resting the head
- Lift one arm and alternate leg as high as you can
- Hold 3-5 seconds
- Repeat opposite side
Add arm or ankle weights and increase length of hold to progress.

- Lie face down on a firm surface
- Lift arms, legs and head off the floor as high as you can
- Hold 5-10 seconds
- Repeat x 20
To make easier: lift either upper or lower body or move through a small range of motion.
To make more difficult: Add arm or ankle weights and increase length of hold, flutter arms and legs in a swimming motion.
Exercise to Prevent Osteoporosis
The most effective time to build bone is pre-puberty. Research has found that jumping has significant protective effects against bone related decline later in life (McKay et al 2005). This research found that only 10 jumps three times per day is adequate to improve bone mineral density. Weight bearing exercise is incredibly important to build bone, especially if your child tends to spend a lot of time in non-weight bearing sports such as swimming or bike riding. To make sure children are getting the benefits of weight bearing exercise, get them hopping, skipping or jumping every day.
References:
- https://osteoporosis.org.au/
- McKay H.A., MacLean L., Petit M., Mackelvie K., O’Brien K., Janssen P., Beck T., Khan K.M. (2005) ‘Bounce at the bell’: a novel program of short bouts of exercise improves proximal femur bone mass in early pubertal children. British Journal of Sports Medicine 39, 521-526
- Sanders KM, Watts JJ, Abimanyi-Ochom J, Murtaza G. Osteoporosis costing NSW & ACT: A burden of diseaseanalysis – 2012 to 2022. Osteoporosis Australia 2017 ISBN 978-0-9923698-2-8
- Watson, S. L., Weeks, B. K., Weis, L. J., Harding, A. T., Horan, S. A., & Beck, B. R. (2018). High‐intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: the LIFTMOR randomized controlled trial. Journal of Bone and Mineral Research, 33(2), 211-220.

