Our bones are a living tissue and continue to break down and rebuild all the time. Osteoporosis (defined as a condition in which bones become fragile and brittle (1) can occur when bones lose minerals such as calcium, more quickly than the body can replace them. In the picture below you can see as our bone density reduces, the bones become more fragile and we are at a much higher risk of sustaining a fracture.
What we Cannot Change:
Your family history:
Our bone strength is strongly inherited. If one or both of your parents have been diagnosed with osteoporosis or sustained a fracture (as a result of a minor incident) it is worth discussing your bone health with your GP (1).
Your medical history:
- The use of corticosteroids, when taken for long periods (commonly used for asthma, rheumatoid arthritis, coeliac disease and other inflammatory conditions)
- Low hormone levels: (Women) low oestrogen and early menopause, (Men) low testosterone. For more information please see our article on menopause and the musculoskeletal system. https://www.ajphysio.com.au/menopause-and-the-musculoskeletal-system/
- Thyroid conditions: over active thyroid or parathyroid
- Some chronic conditions: Rheumatoid Arthritis, Chronic liver or kidney disease
- Some medicines for epilepsy, breast cancer, prostate cancer and depression. (1)
What we Can Control:
Exercise:
Exercise is one of the primary modifiable factors, capable of influencing bone health by preserving bone mass and strength (5). Exercise maintains bone health into adulthood and helps prevent or slow bone loss after menopause (1). Improving balance and coordination is important in the elderly to reduce the risk of falls (1).
For adults, a combination of progressive resistance training and moderate to high impact weight bearing activities are the most effective ways of preventing bone loss as we age. The activity needs to place some ‘stress’ on the bone to achieve the benefits to our skeletal system. (Some examples include – running, jumping, skipping and brisk walking up a staircase or walking over uneven terrain).
While swimming and cycling are great for our cardiovascular system, they have not been shown to improve our bone density (1). In a systematic review conducted by a group of Brazilian Rheumatologists in 2016, they looked at the evidence over the course of 10 years to see the impact of bone mass in swimming and cycling. The evidence suggests that swimming and cycling do not cause positive effects on bone mineral density. 10 studies linked professional cyclists to having low bone density and 18 studies revealed swimming has no positive effect on bone density. Therefore these are not the most suitable types of exercise if your goal is to improve bone mass and minimise your risk of osteoporosis (8).
For more information on exercise prescription in protecting your bones long term, please read our article The Importance of Exercise in Osteoporosis.
Your calcium intake:
To optimise our absorption of calcium, the evidence suggests that it is best to aim for a calcium rich diet rather than being reliant on calcium supplementation. Some people can experience gastrointestinal upset particularly constipation with calcium supplements. In addition, some evidence suggests there is a slight increased risk of heart attack and possibly stroke with the incorrect use of calcium supplementation (6). Therefore, it is always best to get your calcium through your diet, unless otherwise prescribed by a doctor.
Osteoporosis Australia recommends 3-5 servings of calcium in your diet each day. The number of servings will depend on the types of calcium rich foods (1). While milk, cheese and yoghurt are fantastic sources of calcium, If you have a lactose intolerance or dislike dairy, other calcium rich sources include tinned sardines and salmon, almonds, dried figs and apricots, leafy green vegetables such as bok choy, silverbeet, kale and spinach. In addition chickpeas, tahini, and tofu are other sources to consider.
It is important to remember that in order for our bodies to appropriately absorb the calcium intake through our food, we need to have the appropriate Vitamin D levels, and minimise excessive caffeine and alcohol intake.

Your vitamin D:
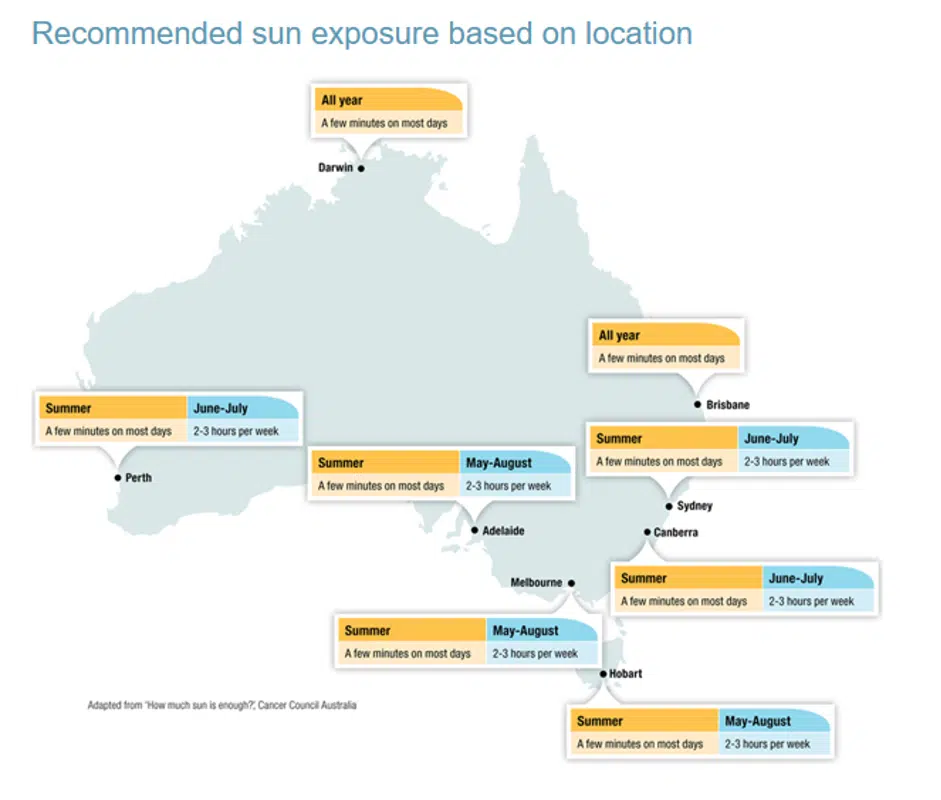
Vitamin D is made in the skin when exposed to sunlight. Vitamin D deficiency is more common in a frail and elderly patient population who receive limited sunshine (6), and often very uncommon in Australia where we spend a lot of our time outdoors (1). The current conservative recommendations are to obtain daily morning sunshine for about 20-30mins (1). Supplementation should only be considered when your Vitamin D level is measured as low through a blood test (6).
Other Lifestyle factors:
Minimising excessive alcohol intake and smoking are important lifestyle strategies to protect our bones long term (1).
Summary: How can I strengthen and look after my bones long term?
- Some factors will impact on our bone health that we are unable to control (medical conditions, certain medications and family history)
- Exercise is vital in maintaining healthy bones. Exercise incorporating moderate to high impact activities improves muscle strength and bone density.
- Consume 3-5 servings or calcium through your diet each day, rather than being reliant on supplementation.
- Vitamin D supports calcium uptake in our bones. It is recommended to aim for 20-30 minutes of morning sunshine daily
- Minimise excessive alcohol consumption and consider finding to support to quit smoking
Where to From Here?
If you are keen to know more about Osteoporosis and what you can do to protect your bones see the Osteoporosis Australia website or phone Osteoporosis Australia on 1800 242 141.
If you think you might be at risk of osteoporosis, your bone density can be measured through a Bone Mineral Density Scan (DEXA). It is a quick painless, safe and simple test. Only a small dose of radiation is used and you lie on a bed fully clothed. You can organise a DEXA scan by talking to your GP (3).
In addition, our expert team at SPC offers personalised assessments for exercise prescription/therapy and small group classes called ‘bone builders’ designed by Physios. If you’re time poor and can’t make it into the clinic you can access advice via telehealth and exercise via our online classes. It is important to consider your bone health now to minimise your risk of sustaining a fracture or break in years to come.
References:
(1) Osteoporosis Australia, What you need to know about Osteoporosis – Consumer Guide, 4th Edition (2017).
(2) Australian Institute of Health and Welfare, Australian Government – Osteoporosis Web Report (2020).
(3) American Bone Health, Medication that can be bad for your bones: https://americanbonehealth.org/bone-health/medications-that-can-be-bad-for-your-bones-2/ (2019).
(4) Osteoporosis Resources, Garvin Institute of Medical Research: https://www.garvan.org.au/research/diseases/osteoporosis/about
(5) Exercise and bone health across the lifespan, Biogerontology, 18, 931-946 (2017)
(6) Reid, I., & Bollard, M. (2019). Controversies in medicine: the role of calcium and vitamin D Supplements in adults. Medical Journal of Australia. 211 (10).
(7) The Economic Times, Not Just for Bones – Calcium is crucial for cardiac functioning too. (2018). https://economictimes.indiatimes.com/magazines/panache/not-just-for-bones-calcium-is-crucial-for-cardiac-functioning-too-heres-how-to-ensure-youre-never-deficient/articleshow/64272449.cms
(8) Abrahin, O., Rodrigues, R., Marcal, A., Alves, E., Figueiredo, R., Sousa, E. (2016). Swimming and cycling do not cause positive effects on bone mineral density: a systematic review. Revista Brasileira de Reumatologia (English Edition). 56(4), p345-341.

