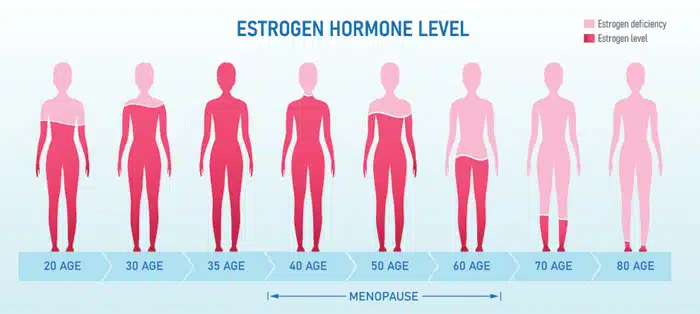
Whilst we all get aches and pains from time to time, they become significantly more frequent as a woman goes through menopause. This occurs because oestrogen directly affects the structure and function of bone, muscle, tendon and ligaments (1). Therefore, the hormonal changes of menopause, where there is a reduction in oestrogen, has a significant impact on musculoskeletal function. An understanding of these changes by all women is paramount, as much can be done prior to, during and after menopause, to minimise the effects these changes have on our body and the subsequent impact they have on one’s quality of life.
How does Menopause Affect our Muscles?
With the decline in oestrogen at menopause, women experience a rapid decrease in muscle mass and strength (1,2) and are more prone to muscle injury (1, 2). This affects all skeletal muscles within the body and might explain why a woman may start to develop more muscular injuries or aches and pains, whilst participating in their regular activities as they approach menopause. It might also explain why the distance you are able to hit your golf ball has suddenly started to decrease!
As these changes affect all skeletal muscles, our pelvic floor muscles are also impacted. Many women have an underlying weakness in their pelvic floor muscles, often existing from obstetric injury during childbirth or a chronic history of constipation or coughing, therefore it is often during menopause that they develop symptoms of urinary or faecal incontinence relating to pelvic floor muscle weakness.
Additionally, oestrogen regulates the production of cortisol, a stress hormone, in the body. When oestrogen levels drop, the cortisol levels are increased (3). These higher levels of cortisol can cause the muscles to become tense and painful, as cortisol makes you more sensitive to pain. Subsequently, women can develop aching muscles, even in the pelvic floor where pelvic floor muscle tension can cause pelvic floor muscle dysfunction and pain.
How does Menopause Affect our Ligaments and Tendons?
Within the musculoskeletal system, ligaments and tendons function as connective tissue. Ligaments attach bone to bone and tendons attach bone to muscle. Oestrogen reduces the collagen content of connective tissues, increasing the stiffness in the ligaments and tendons. (1,2) In the case of ligaments, a stiffer ligament is preferable, as it helps to maintain joint stability and prevent injury. However, a stiffer tendon is not necessarily beneficial. A stiff tendon will not stretch, therefore the muscle attached to that tendon will experience more eccentric loading, often resulting in muscle injury and tendinopathies (1, 4). In women, these commonly affect the gluteal, hamstring, achilles and rotator cuff tendons resulting in aching in hips, bottom, heels and shoulders.
How does Menopause Affect our Bone Health?
Maintaining strong, healthy bones is essential for everyone of all stages of life. Bones are a living tissue and constantly changing and remodelling, as new bone is made, and old bone is broken down. In childhood and early adulthood, your body makes new bone faster than it breaks down the old bone, therefore your bone mass increases. At around the age of 30, most people reach their peak bone mass and after this time, the amount of bone loss starts to increase more rapidly, reducing our overall bone mass. In women, the reduced oestrogen levels associated with menopause leads to a further loss in bone density. It is estimated that on average, women lose up to 10 % of their bone mass in the first 5 years after menopause (5). Subsequently, women are at a greater risk of developing osteoporosis, a condition in which bones become thinner and more brittle and may fracture more easily. In fact, the lifetime risk of sustaining an osteoporotic fracture after 50 years is close to 50% for women and 20% for men (6). To help reduce your risk of developing osteoporosis it is important to prevent bone loss.
How do we Minimise the Impacts of Menopause on our Musculoskeletal System?
Exercise is the most effective lifestyle strategy to maintain healthy bone and muscle. A combination of both progressive resistance training and moderate impact weight bearing exercises can assist in improving and maintaining bone density as well as increasing muscle mass and strength.
Current World Health Organisation Guidelines recommend that adults complete 150 minutes of moderate intensity exercise each week in addition to 2-3 resistance training/strength sessions. This equates to approximately 30 minutes of exercise per day. Exercise also provides both cardiovascular and mental health benefits.
Given that musculoskeletal symptoms are common and can vary widely between individuals, it is important to consult your GP or Physiotherapist to formulate an individualised management program to optimise your long-term musculoskeletal health and quality of life. In fact, even prior to menopause, it is helpful to build up our bone and muscle stores so that the additional decline associated with menopause is less impactful.
At Sydney Pelvic Clinic we provide a tailored management plan based on your symptoms and goals. We provide manual therapy, education and targeted exercise programs which are individually tailored to each person’s needs. These include specialised Bone Builder sessions to specifically target bone health for those with low bone density (osteopenia) or osteoporosis. It is extremely important that any exercise program be targeted to an individual’s needs to ensure that the musculoskeletal system is adequately challenged without overloading it and increasing injury risk.
Read Part 2: Menopause & Pelvic Floor Health
References:
- Chidi- Ogbolu N & Baar K 2019, ‘Effect of Estrogen on musculoskeletal performance and injury risk’, Frontier in physiology, vol. 9, article 1834.
- Nedergaard A, Henriksen K, Karsdal MA & Christiansen C (2013), ‘Menopause, Estrogens and frailty’ Gynecological Endocrinology, vol. 29, no. 5, pp 418-423.
- Woods NF,Mitchell ES & Smith- DiJulio K 2009, ‘Cortisol levels during the menopausal transition and early postmenopause: Observations from the Seattle Midlife Women’s Health Study’, Menopause, vol. 16, no. 4, pp. 708-718.
- Rees JD, Maffuli, N & Cook, J 2017, ‘Management of tendinopathy’, The American Journal of Sports Medicine,vol. 37, no. 9, pp. 1855-1867.
- Australasian Menopause Society 2020, www.menopause.org.au
- Rizzoli R 2018, ‘Postmenopausal osteoporosis: Assessment and management’ Best Practice & Research Clinical Epidemiology & Metabolism, vol. 32, no. 5, pp. 739-757.


