Most Australian women experience menopause between the ages of 45-55 years, with an average age of approximately 51. Menopause comes with a myriad of symptoms such as hot flushes, night sweats, whole body aches and pains, fatigue and irritability. However, beyond these noticeable changes, menopause also significantly affects pelvic health, bone health as well as the health of our muscles, fascia and tendons.
An understanding of these changes by all women is paramount, as much can be done prior to, during and after menopause to minimise the uncomfortable and often hidden symptoms of menopause.
What is Menopause?
Menopause marks the end of a woman’s reproductive life and specifically refers to the final menstrual period that a woman experiences. At menopause, ovulation no longer occurs and the production of oestrogen and progesterone declines.
Menopause is Often Considered in Stages:
- Perimenopause – the time leading up to menopause when a woman may start to experience a variety of symptoms; these are a result of fluctuations in hormone levels.
- Menopause -The time when the final menstrual period occurs.
- Postmenopause – Starts when a woman has had no menstrual period for 12 months.
And Symptoms of Menopause
Symptoms of menopause start to occur during the perimenopausal period due to fluctuations in oestrogen and progesterone levels. These symptoms often last for 4-8 years, but are typically more frequent and intense around the final menstrual period. Symptoms will present differently from woman to woman and, due to the large role oestrogen and progesterone play in our bodies, can affect multiple bodily functions and systems.
Symptoms may include:
- Hot flushes/night sweats
- Menstrual changes – irregular bleeding, changes in flow
- Whole body aches and pains
- Fatigue
- Irritability
- Sleep Disturbances
- Anxiety and Depression
- Low libido
- Pelvic symptoms
Menopause and the Pelvic Floor
Vaginal health is an essential component to healthy aging for all women. Oestrogen plays an important role in keeping the tissues of our vulva, vagina, bladder and pelvic floor muscles strong and flexible. When oestrogen levels drop due to menopause, it is common for women to experience pelvic symptoms, particularly genitourinary symptoms. These symptoms previously known as Atrophic Vaginitis or Vulvovaginal Atrophy (VVA), have in recent years been renamed ‘Genitourinary Syndrome of Menopause’ (GSM) to more accurately reflect the multiple changes that occur during menopause.
What is Genitourinary Syndrome of Menopause (GSM):
GSM is a term used to describe the multiple anatomical and functional changes that affect the external genitalia, vagina, bladder, urethra and pelvic floor tissues which occur at menopause.
Why does GSM occur?
The vagina, vestibule of the vulva, urethra and bladder all contain high levels of oestrogen receptors. As oestrogen levels decline with menopause, the tissues of the vulva, vagina and urethra can become thinner and lose their elasticity, there is a reduction in lubrication of the vagina and the pelvic floor muscles also become thinner and less flexible.
What are the symptoms of GSM?
- Vaginal/Vulval symptoms:
- Dryness
- Burning/itching
- Vaginal shortening and narrowing
- Bladder symptoms:
- Urinary Urge
- Urinary Incontinence
- Bladder infections
- Recurrent urinary tract infections
- Stress Urinary Incontinence
- Pain with urination (Dysuria)
- Sexual symptoms:
- Pain or discomfort with sexual intercourse (Dyspareunia)
- Loss of libido
- Heaviness:
- Pelvic organ prolapse
With Menopause, bowel symptoms such as the inability to control wind and faecal incontinence may also be present. This is due to pelvic floor muscle weakness caused by oestrogen loss. These symptoms are more common in women with an underlying weakness in their pelvic floor muscles, possibly caused by obstetric injury during childbirth or a chronic history of constipation or coughing.
It has been reported that genitourinary symptoms of menopause are bothersome in more than 50% of postmenopausal women. Unfortunately, due to the sensitive nature of symptoms, or perhaps lack of awareness of treatment options, women may not seek medical assistance. In contrast to the menopausal hot flushes and night sweats which ease and cease over time, pelvic symptoms persist or continue to progress.
Given that these pelvic symptoms persist or continue to progress, it is important to consult your GP or Pelvic Physiotherapist to formulate an individualised management program to optimise your long- term pelvic health and quality of life.
At Sydney Pelvic Clinic we provide a tailored management plan based on your symptoms and goals. This can include pelvic floor muscle retraining, bladder training and providing guidance on lifestyle factors to assist in minimising symptoms.
Whilst it is never too late to address these symptoms, consulting a Pelvic Physiotherapist prior to menopause can assist in ensuring optimal pelvic function is maintained for longer and minimise future symptom development.
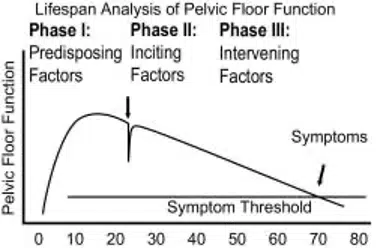
DeLancy et al 2008 Life span model of pelvic floor function.
Pelvic health is like a bank account. Throughout life we should be investing in our pelvic health by making small deposits, ensuring function and that the pelvic floor muscles remain strong. With the onset of menopause, we start to make small withdrawals, regularly. Consider that if over time you have invested enough in maintaining your pelvic floor, small withdrawals will not affect your overall function. However, if your pelvic floor reserve was low prior to menopause, then you will start to experience symptoms earlier, upsetting the balance of your pelvic health.
Read Part 1: Menopause & The Muskuloskeletal System
References:
DeLancey JOL, Low LK, Miller JM, Patel DA &Tumbarello JA (2008), ‘Graphic integration of causal factors of pelvic floor disorders: an integrated life span model’, American Journal of Obstetrics & Gynaecology vol. 199 pp 610.e1-610.e5.
Farrell E (2017), ‘Genitourinary syndrome of menopause’, Australian Family Physician vol. 46, no. 7, pp. 481-484.
Nappi RE, Martini E, Cucinella L, Martella S, Tiranini L, Inzoli A, Brambbilla E, Bosoni D, Cassani C & Gardella B (2019), ‘Addressing vulvovaginal atrophy (VVA)/Genitourinary Syndrome of Menopause (GSM) for healthy aging in women’, Frontiers in Endocrinology vol. 10, p. 561. Doi:10.3389/fendo.2019.00561.
Helpful websites:
https://www.jeanhailes.org.au/resources/menopause-fact-sheet
https://www.menopause.org.au

