Endometriosis is derived from the Latin term endo ‘inside,’ metra ‘uterus’ and osis ‘disease.’ It is a complex, inflammatory, estrogen dependant pain disorder affecting 11% of women, girls and those assigned female at birth. It is characterised by tissue similar to the lining of the uterus (endometrium) growing in other parts of the body, including around the bladder, bowel and it has also been found in the skin, lungs and brain. The most common symptoms of endometriosis are period pain (dysmenorrhea), heavy bleeding and fatigue. It takes an average of 6.5 years to receive a diagnosis of Endometriosis, and by this point, a person’s pain experience is not accurately represented by the stage of disease. Meaning women with stage 4 endo can experience minimal symptoms, where others with stage 1 can be immensely impacted by pain. It can be a confusing experience for women to undergo laparoscopic surgery, where all diseased tissue has been successfully removed, yet their pain persists. This article seeks to explain the broader, non-lesion contributors to pain and empower you with ways to address them.
Endometriosis-associated pain (EAP) syndrome
EAP syndrome is defined by European Guidelines for Chronic Pelvic Pain as ‘persistent or recurrent pelvic pain in patients with laparoscopically confirmed endometriosis, and the term is used when the symptoms persist despite adequate endometriosis treatment. It is often associated with negative cognitive, behavioural, sexual or emotional consequences, as well as with symptoms suggestive of lower urinary tract, sexual, bowel or gynaecological dysfunction.’
While Endo is thought to initially arise due to local inflammation, lesions and hormonal effects, the persistent nature of EAP is due to a more widespread response in the body. This response includes changes in the central and peripheral nervous system, pelvic organ cross talk, changes in the pelvic floor and abdominal muscles, alterations in mood, stress and sleep and the presence of comorbid pain syndromes.
Central and peripheral sensitisation
Research has shown increases in pelvic nerve size, density, and activity levels in people with EAP. This means nerves in the pelvis become excitable and send more messages to the brain. This neural excitability is not due to Endo lesions, but more of a widespread sensitised state – like when an alarm goes off without a well-defined cause. Over time, this causes the brain to be bombarded with nerve signals from the pelvic region, and it loses its ability to dampen down the ‘noise’ from below. When we are in this sensitised state, our pain threshold reduces throughout our whole body, meaning we are more sensitive to light, sound, touch, temperature, and smell. It can also lead to interpreting normal bodily sensations as a threat and may cause discomfort with digestion or bladder filling. When amplification of normal internal sensations causes internal pain, this is referred to as visceral hypersensitivity.
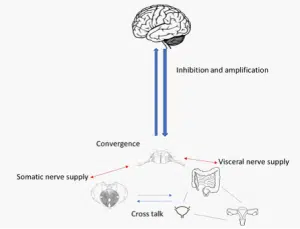
Pelvic organ cross-talk
The pelvis is a busy area, housing the bladder, bowel, sex organs, pelvic joints and muscles. All these structures are connected by nerves, which share similar pathways on the spinal cord before travelling up to the brain. When one area becomes sensitive, resulting in an increase in nerve action, it easily spreads to another area, causing it to become excited or sensitive. This ‘cross-talk’ is one of the main reasons our bladder, bowel and pelvic muscle function is often affected with EAP.
Pelvic floor and abdominal muscle function
Research has shown that women with EAP are more likely to have tight pelvic floor and abdominal muscles. In fact, 45% of Endo patients are not able to relax their pelvic floor muscles. This is called pelvic floor tension myalgia – where the pelvic floor muscles are tight and painful to touch. Symptoms of pelvic floor tension myalgia are pain with penetrative sex (dyspareunia), genital aches or sharp pains, difficulty or pain with emptying the bladder (dysuria) or bowel (dyschezia).
Alterations in mood, stress and sleep
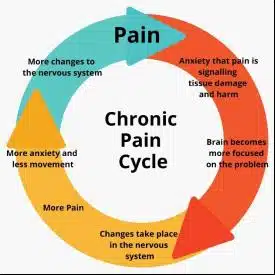
Research has shown a depressed mood, anxiety, poor sleep quality, pain anticipation and catastrophising, stress and increased attention to pain are all associated with higher pain intensity. This relationship with these factors and endometriosis is thought to be bi-directional, meaning endometriosis and inflammation can alter mood, while stress/anxiety and maladaptive pain beliefs can amplify EAP. This is often referred to as the vicious cycle of pain and explains why its important to address the psychological and emotional distress often experienced in EAP.
Co-existing pain conditions
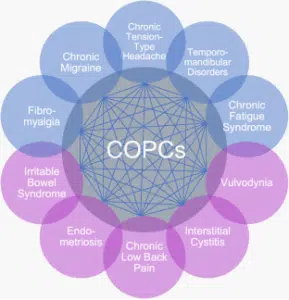
Women with endometriosis are far more likely to experience additional chronic overlapping pain conditions, such as bladder pain syndrome (BPS). In fact, 40 – 60% Endo patients are thought to have co-existing BPS which is characterized by urinary urgency and frequency. The rate of irritable bowel syndrome (IBS) for women with EAP is 60% and 11% have co-existing vulvodynia. All these conditions share a common casual pathway of increased levels of sensitization, inflammation, and a consequent reduction in quality of life.
Chronic overlapping pain conditions
https://chronicpainresearch.org/about_copcs/
Although this presents a complex picture for EAP syndrome, with many different factors beyond lesions influencing one’s pain experience, it is important to remember your body is capable of change at any point in your journey. The key is to identify what factors are influencing you and work with a team of skilled and supportive healthcare professionals to help you manage them. Your EAP toolkit often includes movement and exercise therapy, mindfulness and stress reduction, pelvic physiotherapy, dietary changes and psychology. Overtime, this broader, more holistic approach, can reduce pain and improve the quality of your life.